Leukemia is cancer of the white blood cells. White blood cells, which are also called leukocytes, fight against infections and other diseases. In leukemia, the bone marrow produces many abnormal white blood cells, and these abnormal white blood cells enter the bloodstream by filling the bone marrow. Unlike healthy white blood cells, these cannot protect the body from infections. Leukemia is the most common type of cancer amongst children.
What are the Types of Leukemia?
There are many different types of leukemia. The most common type in children is Acute Lymphocytic Leukemia, ALL for short. Less common types of childhood leukemia can be listed as Acute Myeloid Leukemia, Chronic Myeloid Leukemia (CML) and Juvenile Myelomonocytic Leukemia.
What are the Signs and Symptoms of Leukemia?
Because their white blood cells cannot fight against infections, children with leukemia may get more viral or bacterial infections compared to other children. In addition, anemia or exsanguinity is also often common. Other symptoms of leukemia are: anemia, pale appearance, pain in bones or joints, swollen lymph nodes (swollen glands) in the neck, loss of appetite, weight loss, irresolute fever, the body getting bruised easily, nosebleeds, swelling in the gums.

How is Leukemia Diagnosed?
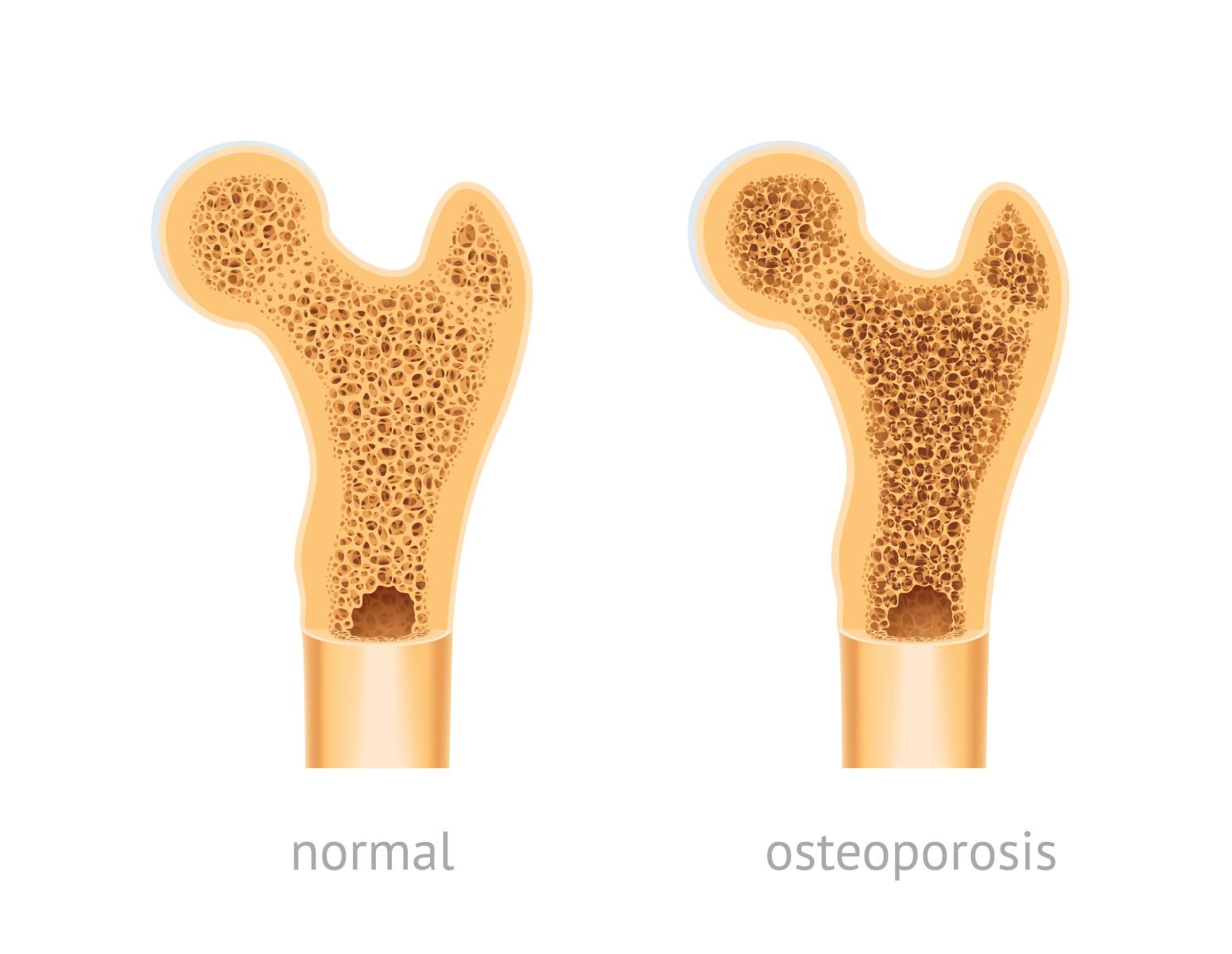
The steps followed to find out if a child has leukemia can be summarized as follows; the physician first asks questions about the symptoms. Then, they examine them to check for signs of infection, anemia, unusual bleeding, and swollen lymph nodes. In addition to this examination, some tests may be requested. Depending on the results, other tests such as bone marrow biopsy, spinal needle to obtain lumbar fluid, imaging tests, genetic tests may also be performed.
How Is Leukemia Treated?
A pediatric oncologist (a doctor who specializes in childhood cancer) leads the medical team caring for the child with leukemia. The oncologist works together with other specialists, including nurses, social workers, psychologists and surgeons. The main treatment approach in childhood leukemia is chemotherapy. The doses and drugs used may differ depending on the child’s age and the type of leukemia. Other treatment methods such as radiation therapy, targeted drugs, bone marrow transplantation can also be performed.

Some other facts about leukemia:
- Your child’s sex can affect your prognosis and how long your treatment will take.
- Bone marrow transplantation is not always needed when treating leukemia. This depends on the type of leukemia and the response to treatment.
- You should take fever very seriously during leukemia treatment. In most cases, the use of antibiotics should be started immediately.
- You may need to interrupt your child’s vaccinations for a while during the treatment for leukemia.
- There may be many long-term side effects associated with leukemia treatment. Depending on the treatment your child receives, post-treatment follow-up is required.